Oct 30, 2020
Caring for our smallest babies
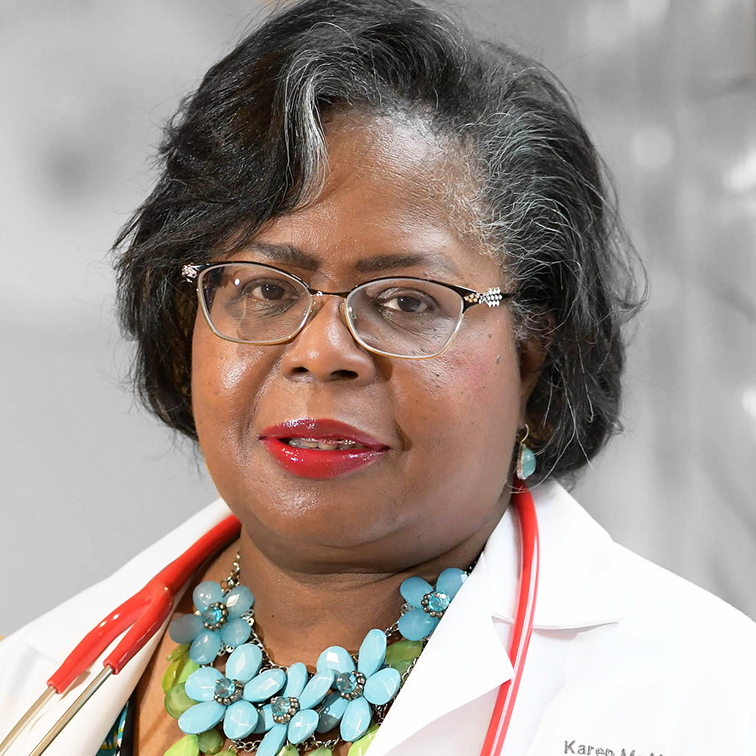
Coverage is proud to publish columns featuring the perspectives of Black women physicians who belong to the Diva Docs network in Greater Boston. Today, Dr. Karen McAlmon, neonatologist at Winchester Hospital and Beth Israel Deaconess Medical Center and director of the Beth Israel Lahey Neonatology Network, shares her thoughts with Dr. Philomena Asante, leader of Diva Docs Boston and creator of the Diva Docs series for Coverage.
I was born in Brooklyn, N.Y., the daughter of immigrants from Panama. We had no physicians in the family – in fact, we didn’t even go to the doctor very often. My parents cared deeply about education and I was a bookworm who thought I might be a teacher. I earned a scholarship from a program called A Better Chance, which sends students of color to independent or suburban public schools – in my case, Concord Academy, which opened my eyes to the world’s possibilities. From there, I went to Stanford University, where I fell in love with science. I volunteered at the Lucile Packard Children’s Hospital, and realized I could combine my desire to teach, my love for science, and my interest in working with children by becoming a physician. I then attended Harvard Medical School, where I found I really liked neonatology.

Neonatologists are pediatricians who specialize in the care of newborns, especially those who are born before their due date, even as young as 22 or 23 weeks. We care for them until they leave the hospital, sometimes for months.
Neonatologists care not only for the newborn, but the whole family at a time when things are critical and you can make a real difference. The greatest joy is being able to send a baby home healthy, with the expectation that they’re going to have a productive life.
However, there is more death in neonatology than almost any other specialty in pediatrics. Yet, I’ve learned that you can make a difference for every baby. We, the medical team, are often the only people other than the parents who know that baby during his or her lifetime, no matter how short, and that gives us a bond, a bond that is lasting.
How racism impacts our smallest babies and their mothers
In neonatology, like nearly every other area of medicine in the U.S., there are racial disparities. These are not inequities caused by race, but rather by racism.
In this country, racism has resulted in segregation, restricted access to housing, healthy food, employment, education and health care. These are what we call “social determinants of health,” factors that can be associated with physical and mental health conditions. The stress of racism itself also leads to physiologic effects that have been described as “weathering,” which can lead to a shorter lifespan.
Researchers have found disproportionately adverse outcomes including low birth weight and preterm delivery in Black women even when access to care is equal. Black women with similar income and professions and education as white women their age have faced a hurdle those white women have not: institutional and individualized racism that can cause constant, lifelong, toxic stress. We see higher rates of diseases including hypertension and diabetes among Black women. These can complicate a pregnancy and lead to conditions that threaten a mother’s life and her baby’s life.
Rates of complications of prematurity are higher in Black infants: Black infants have a two-fold greater risk of dying from intraventricular hemorrhage, or brain bleeding, than white infants. A recent study found a higher concentration of intraventricular hemorrhage in newborns in neighborhoods where there were higher concentrations of minorities due to a history of racial segregation policies. In addition, researchers have found a higher incidence of late-onset sepsis, less timely screening for retinopathy of prematurity (a potentially blinding disease caused by abnormal development of retinal blood vessels), and a higher incidence of necrotizing enterocolitis (a devastating disease that affects the intestine) in Black premature infants compared with their white counterparts.
Two factors can help improve outcomes for preterm babies before they’re born: the use of antenatal steroids to help with lung and other organ maturation, and the early use of Cesarean section if a baby is in distress. Historically there was lower use of both in Black women; however, trends now show improvement thanks to better standardization of quality measures and use of best practices. We know training to help clinicians consistently follow standards, regardless of race, can help decrease disparities.

Addressing inequities
In medicine, if you think something is important, you measure it, you track it and you evaluate trends. We need to measure processes and outcomes within neonatology and within all of medicine, stratifying by race. We should have quality improvement measures attached to racial disparities in medicine, and our data should be publicly reported to ensure accountability.
(This year, we are seeing a stark example of how important it is to track disparities with COVID-19, where we have found the population of color is disproportionately at risk.)
In order to effect change, we need to know if there are differences in treatment and outcomes between the general population and the population of color at our hospitals, and where we fall with regard to comparable hospitals.
For example, currently, hospitals are required by our accrediting bodies to track breastfeeding and C-section rates; those rates should be tracked by race as well.
We also know unconscious bias can affect the delivery of health care to people of color. We need to increase the cultural competency of physicians, starting in medical school and continuing in hospitals. Institutions must commit to training all members of medical teams to recognize and prevent implicit bias and to ensure that their staff gives equal care to all who enter and all who need that care, especially the most vulnerable, our babies. Training helps increase understanding, respect and empathy, which strengthen relationships between physicians and parents. That will better enhance the care of babies, and better enable us to form alliances with families to improve the health of babies.
Questions families can ask the first day a newborn is admitted to the NICU
- Who is the physician in charge of my baby’s care? You want to know who that is and you want to be able to speak with them. You want to know how they will communicate with you about your baby’s course of treatment. You want the neonatal team to know that you are engaged and involved, even though you are separated from your baby while they are in the NICU.
- How can I provide care for my baby while he or she is in the NICU? Can I hold my baby, skin to skin, which is known as "kangaroo care"? That has been shown to settle babies, decrease their heart rate, and decrease their respiratory rate. Even very small and very sick babies can have kangaroo care (and both moms and dads can do kangaroo care). How often can I be in the unit? Will I be able to change their diaper and take their temperature? Can I go on rounds?

- What resources are available to help me navigate hospitalization and care for my baby after discharge? Can I speak with a social worker? What are the things I need to prepare for home? What are the services my baby is eligible for?
Having a baby in the NICU is deeply stressful. Parents should know it’s normal to have swings in emotion and to have a sense of grief and loss for the birth experience they expected to have. It’s important to make sure there are supports for the whole family, including older siblings.
Early intervention
Massachusetts has an Early Intervention Program, run through the Department of Public Health, which provides developmental follow-up for babies who are at risk either because of prematurity, substance exposure, or developmental problems due to chromosomal problems or other issues. Until the age of 3, children are eligible for early intervention. The baby is evaluated at their home to determine whether they have needs that could be met by a multidisciplinary team. That team can include a nurse, or an occupational therapist, physical therapist or speech therapist who, for the first year or more, comes into the home, and after age 2, may provide center-based care. This program is accessible to anyone, regardless of income. It is an excellent program that gets children the resources that they need for optimal development.
Going home
As neonatologists, we connect with pediatricians to ensure there is appropriate follow-up care for our babies. There is no greater joy than being able to send a baby home healthy, with the care they need, the care every baby deserves.
PHOTOS OF Dr. McALMON AND Dr. ASANTE BY FAITH NINIVAGGI