Jan 29, 2024
A message for mothers
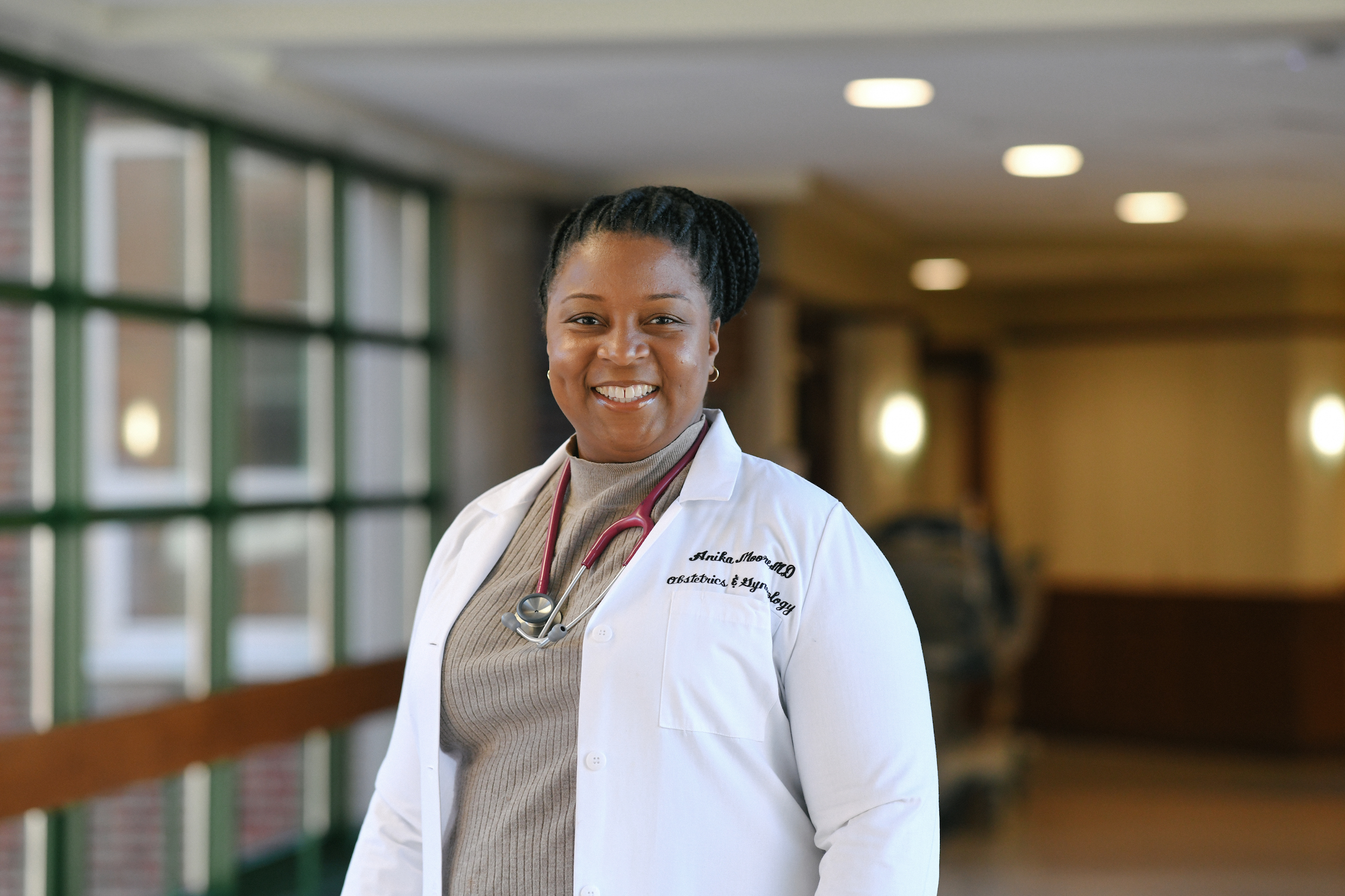
Dr. Anika Moore, an obstetrician, shares her thoughts about women’s health and health disparities with Dr. Philomena Asante, leader of Diva Docs Boston and creator of the Diva Docs series for Coverage.
I was inspired to become an obstetrician by my mother’s obstetrician. He lived in my hometown of Cincinnati, and when I was in high school, I had the opportunity to shadow him for a week as part of a career program. One day, he gave me the opportunity to watch him deliver a baby. It was so powerful. I knew right then that was the path I wanted to follow.
Growing up, my grandmother would always say, “The most important thing you can do is have a heart full of love, a listening ear and a hand willing to help others.” When I decided to go into medicine, as an African-American woman, I promised never to forget my grandmother and to do everything I could to ensure women were treated well -- to listen, partner and connect with women to help take care of their health needs. And that is exactly what I do at Brockton Neighborhood Health Center.
I treat women of all ages, from adolescence through menopause. I treat pregnant women, women with infertility issues, menopausal women, women dealing with endometriosis, and a host of other medical issues. My patients are from all around the world but most of my patients are from Cape Verde, Haiti, and Brazil. I love working with all women regardless of color, class, creed, sexual orientation or identity. I love mentoring, taking care of, teaching, and advocating for women.
There is perhaps no more hopeful, joyful field of medicine than obstetrics. We help bring new life into the world. And yet, in America, the joy of our field is mottled by grim inequities.
The maternal mortality rate in this country has more than doubled in the past two decades, in stark contrast to the rest of the developed world. And the rates are even more alarming for Black women, who are three times more likely to die from a pregnancy-related cause than white women. Black women experience higher rates of infertility, fetal death, maternal death, and preterm birth than white women. The disparities persist across class lines: The pregnancy-related mortality rate among Black women with a completed college education or higher is 5.2 times greater than their white counterparts, and 1.6 times greater than that of a white woman with less than a high school diploma.

There are no genetic reasons Black women should suffer a higher rate of death or complications during pregnancy or childbirth. There are economic factors, employment, housing, and access issues that make many Black women vulnerable to chronic conditions that can lead to high-risk pregnancies. And there is the relentless stress of racism. Importantly, within the health care system itself, as the American College of Obstetricians and Gynecologists has noted in recent years, there are also bias issues. Many of these outcomes could be prevented with better health care, communication and support.
What can women do to protect themselves as well as their babies and have a healthy pregnancy?
First, I tell my patients, become an educated consumer. Be aware of disparities in care. And when you go to get your prenatal care, ask questions:
- What can I do to decrease my risk of maternal mortality?
- What pregnancy symptoms are normal and what’s an emergency?
- How do I contact my provider with questions and health concerns?
- Is there anything about me or my medical history that puts me at increased risk?
- What can I do to decrease my risk?
- Is the labor and delivery team at the hospital associated with this practice equipped to deal with high-risk patients?
- Interview the ob-gyn to make sure you connect with them, that they seem knowledgeable, willing to listen to your concerns, look out for your best interest and take care of you.
- Seek prenatal care early, as soon as you know you’re pregnant. And if you are obese or if you have any chronic diseases like diabetes or hypertension, consider going to an OB/GYN before you get pregnant to figure out what you need to do to prepare your body for the pregnancy and to find out how these medical conditions can affect you. It’s important to manage these conditions because they can increase the risk of maternal mortality.
- While you are pregnant, take prenatal vitamins to make sure you are getting the nutrients you and your baby need. Sign up for prenatal classes and breastfeeding classes, and be actively involved in seeking information about your pregnancy and the child birthing process. Some insurance plans pay for these classes. Ask your local hospital and OB/GYN office about resources in your community. Many towns offer free prenatal classes, breastfeeding classes, and counseling.
- There are four red flags every pregnant woman should be aware of: If you have heavy vaginal bleeding; leakage of fluid; strong abdominal pain, cramping or contractions; or a severe headache that is not relieved with Tylenol, then you need to come in and see your doctor.
- Most importantly, trust your own intuition and intelligence. Don’t be afraid to ask too many questions, and never think you are asking a dumb question. And don’t hesitate to contact your doctor after hours. There’s always someone on call to answer any of your questions or concerns.
But the burden is not just on patients. Clinicians, hospitals and provider practices share responsibility here. What steps can we take to change the maternal mortality trend?
No. 1, we can make a commitment to understanding the cultural, societal, and economic issues that affect health outcomes in minority mothers and babies. We can make sure our staff, including nurses and physician assistants, know the statistics and are educated on how we can do better, through grand rounds, staff meetings and lectures. We can be aware of community resources that can address disparities so we can share that information with patients. And we can increase provider diversity in maternal care.
We also can ensure clinicians and staff are aware of our own biases or at least willing to understand that we may have biases that can affect our interactions with patients, treatment decisions, the willingness of patients to follow our recommendations, and ultimately, patient health outcomes. If our biases cause us to miss opportunities to identify risk factors, or delay in recognizing symptoms, those lapses can have critical consequences for our patients.
As a broader community, we need to understand that this is a problem that cannot to be ignored. We all need to be part of the solution.
Community health centers, local hospitals, public health departments – we can all work together to get the message out that a crisis in maternal health exists. And we can work together to address it.
Did you find this article informative?
All Coverage content can be reprinted for free.
Read more here.
PHOTOS OF DR. MOORE AND DR. ASANTE BY FAITH NINIVAGGI

